Opioids killing First Nations Albertans at disproportionate rates, report shows
'This just tells us that we're not getting on top of it,' says physician from Blood reserve
The death toll from Alberta's opioid epidemic is disproportionately claiming the lives of First Nations people, concludes a new report from the provincial government.
The surveillance study, released Tuesday, showsFirst Nations Albertans are dying from opioid poisoning at a rate three to four times higher than non-First Nations people.
First Nations people account for about six per cent of the provincial population but represent 13 per cent of all opioid poisoning deaths between Jan. 1, 2016 and Dec. 31, 2018, says the report from Alberta Health and The Alberta First Nations Information Governance Centre, a Calgary-based research group.
The report shows 1,957 people died from opioid poisoning in Alberta between Jan. 1, 2016 and Dec. 31, 2018. Of the total, 246 were First Nations people.
The proportion of opioid drug poisonings involving fentanyl increased by more than 80 per cent among First Nations people.
Among First Nations people,carfentanil, methamphetamine and fentanyl saw the largest increases as substances causing drug-poisoning deaths. That coincided with a decrease in overdose deaths caused by prescription drugs such as codeine and benzodiazepines, the report said.
Southern cities hardest hit
Southern Alberta, particularly Calgary and Lethbridge, have been hardest hit by addiction and overdose deaths, the report shows.
The statistics come as no surprise to Dr. Esther Tailfeathers, a family physician from the Blood Tribe First Nation, 220 kilometres south of Calgary.
"It's pretty well known by the people who have been working in the opioid crisis for a while," Tailfeathers said in an interview Wednesday with CBC Radio's Edmonton AM.
"This just tells us that we're not getting on top of it and our problem is moving from our communities into the inner city.
"Even though we're seeing some really positive changes on the Blood reserve, it's definitely not happening with other First Nations because they don't have the resources and they don't have the strategy."
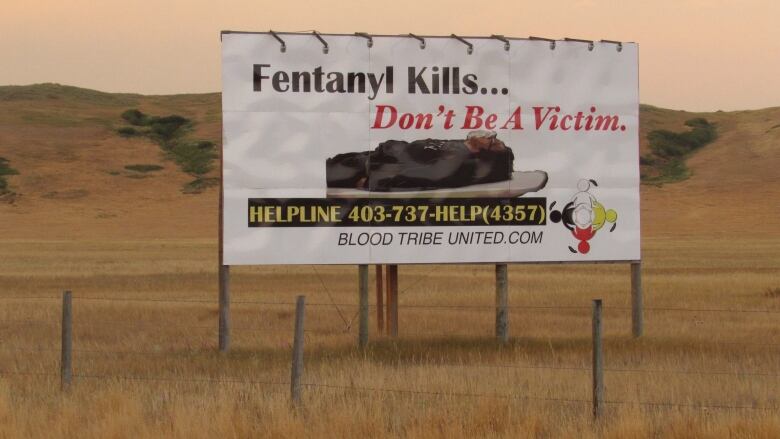
The Blood Tribe community was among the first to raise the alarm about fentanyl in Canada. It was also among the first to take action. It declared a state of emergency in March 2015 after 20 overdose deathsand 60 non-fatal overdoses in a six-month period.
Tailfeathers has lost patients, community members and friends to fentanyl. Her niece died of an overdose in 2017.
Historical trauma, including the painful legacy of residential schools, has contributed to the epidemic, Tailfeathers said.
"It's trauma that has been carried over time through government policy," she said.
"A number of adverse childhood events have affected the mental health of many of our people, so as a result they self-medicate the trauma, the depression and the anxiety and the rest of their mental health problems with alcohol or drugs."
We should have provided supports in the community before we lost our members to death or the streets.- Ester Tailfeathers
Chronic poverty and the isolation of many reserve communities is also to blame, Tailfeathers said. People feel trapped and those most vulnerable to addiction are far removed from the medical care they need.
"Most of our people are living at a $12,000 a year income or less, and we also suffer from poor housing situations across the board."
The report also highlights the demands the opioid crisis has placed on healthcare providers. It examinesdispensing data, emergency department visits and hospitalizations and the number of emergency medical responses to "opioid events."
Ratesfor all the healthcare factors were higher among First Nations people than for non-First Nations people, the report says.
For the years 2016 through 2018, the rate of First Nations people hospitalized for drug use increased more than for other people living in southern Alberta.
The rate of EMS calls to opioid-related events among First Nations people was 31 times higher in Lethbridge than in Red Deer, where the highest rate of response among non-First Nations people was recorded.
'We've been set up for this'
The report notes that during the 36-month study period, the rate of opioid dispensing from community pharmacies decreased 13 per cent among First Nations people, and 11 per cent among non-First Nations people.
"However, the rate of opioid dispensing from community pharmacies has consistently been approximately two times higher among First Nations people compared to non-First Nations people," it says.
Tailfeathers said that is at the root of the problem: First Nations people have been over-prescribed by doctors.
"Most of our people have not enjoyed primary care being given to them or provided in their community. They usually have to travel to the nearest town or city to get primary care.
"And those physicians do not understand the history of the community so our people are prescribed prescription opioids.
"We've been set up for this opioid crisis and that's why you're seeing such a high number of Indigenous people addicted to opioids."
- Drug dealers banned from Blood reserve still know when and how to strike
- Canada's largest First Nation enforces no-trespass bylaw amid fentanyl crisis
Tailfeathers said programs that focus on harm reduction, including naloxone treatment and safe-withdrawal programs, have saved lives on her reserve.
But in their attempts to rid their community of drugs,community leaders have made tough decisions with dangerous and unforeseen consequences, she said.
Banishing drug dealers from the reserve was bad call, she said.
"The decision by our community to ban dealers, mostly to evict people from homes where drug activity happening, was a very poor decision.
"We had an exodus of people that left our community and now are vulnerable in cities like Lethbridge and Calgary.
"They become homeless, they become more involved in the culture of people that are addicted and we don't bring them home.
"We should have provided supports in the community before we lost our members to death or the streets."
With files from Ariel Fournier












_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)



























































































