1 year into the pandemic, Manitoba has Canada's 2nd-worst coronavirus death rate
During the 2nd wave, no other province was worse at preventing COVID-19 deaths

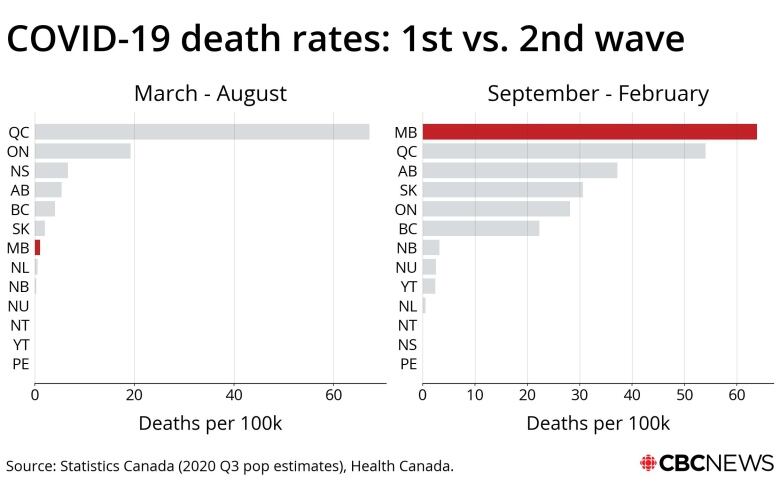
If the ultimate measure of success during a pandemic is how well you prevent your citizens from dying, Manitoba has the second-worst record in Canada.
One year into the declaration of the global pandemic, 66 out of every 100,000 Manitobans have died of COVID-19. Only Quebec, where 124 of every 100,000 residents have died from the disease, owns a more ignominious record.
If you prefer to measure the COVID fatality rate on the basis of deaths per positive case, Manitoba also comes in second-last.
Since the start of the pandemic, 2.8 per cent of Manitobans diagnosed with COVID-19 have succumbed to the disease. Only in Quebec, where the fatality rate is 3.6 per cent, is a COVID diagnosis more likely to translate into a death sentence.
Manitoba's poor performance is no mystery to the official who's served as the face of the province's pandemic fight.
"This is mostly due to having the virus in the long-term care facilities," said Dr. Brent Roussin, chief provincial public health officer, mincing zero words in an interview earlier this week.
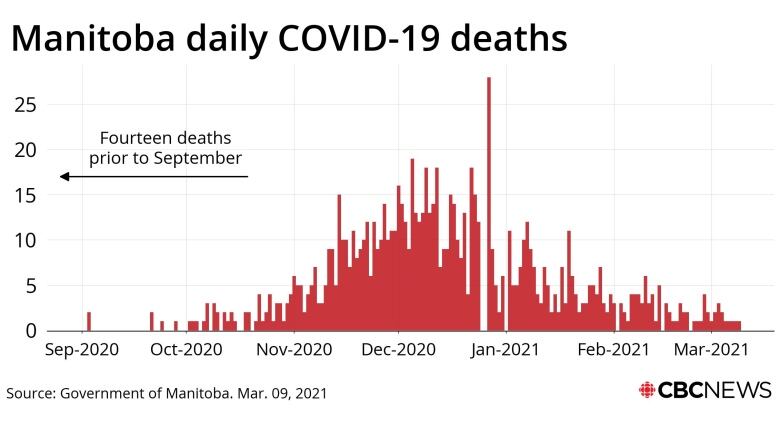
"Roughly half of our deaths that occurredrelated to personal care homes. So I think it wasquite, quite tragic that in our sort ofpeak of that second wave, we had such widespread community transmission that the virus was introduced so many times into these facilities."
That transmission was so widespread,Manitoba actually had the worst COVID fatality rate among Canadian provinces during the second wave of the pandemic,a CBC News analysis revealed.
Manitoba's firstwave was more of a ripple. During the first six months of the pandemic, the disease largely passed over this province.
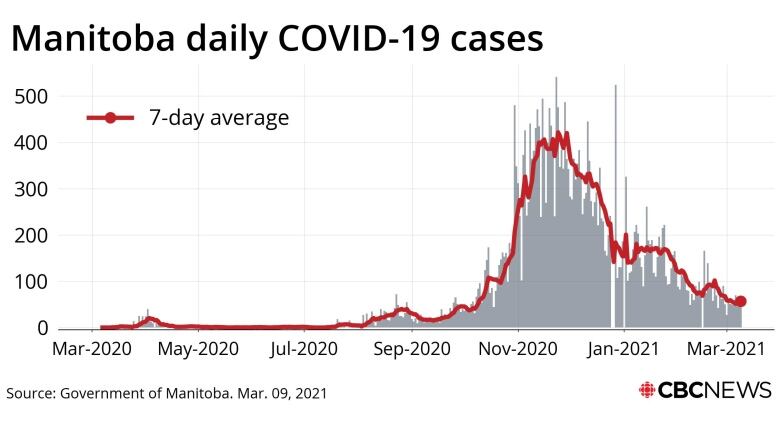
From March 11 to Aug. 11, 2020, only 578 Manitobans were diagnosed with COVID-19; eight of them died.
During the ensuing seven months, another 31,843contracted the diseaseand 900of them died.
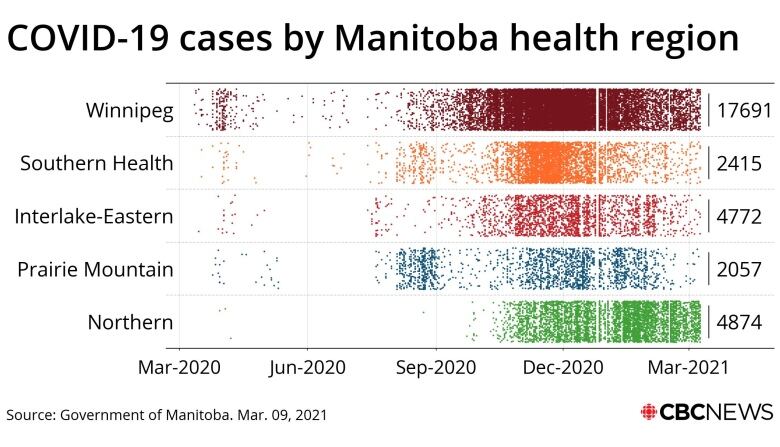
This lopsided pandemic performance was the result of runaway transmissionduringthe fall, primarily in the Winnipeg health region.
After a relatively uneventful summer, which included a 13-day stretch in July without a single new case, Winnipeggers in particular may have been lulled into a false sense of security abouta highly communicable virus.
"I think people were kind of still riding that low of general cases that we had had up that point and probably were not quite following [rules] quite as strictly as they needed to," said Michelle Driedger, a University of Manitoba community health sciences professor who studies public-health communications.
In August, a spike of cases in western Manitoba, centred upon communal living clusters,appeared to be controlled by contact tracing and a mask mandate across the Prairie Mountain Health region.
Similar measures proved unsuccessful in Winnipeg.
When cases started spiking in Manitoba's capital in September, the demand for COVID swabs exceeded the capacity at testing centres. In October, contact tracers could not keep pace with the rising caseload, which was not confined to easily identifiable clusters.
By the middle of October, COVID-19 cases were growing at a rate that exceeded the worst of Manitoba's pandemic scenarios. By November,the virus was effectively omnipresent.
At this point,the firewalls erected around personal care homes which includedno-visitation rules, screening proceduresand attempts to restrictworkers to one facility proved ineffective at preventing outbreaks within those facilities.
"It just does not work to simply try to protect the vulnerable," Roussin said. "When you get widespread community transmission, it's going to get everywhere.
"When you have this, you have to do whatever you can to bring down that community transmission. Andunfortunately, with this virus, that often meant having real strict sort of economic restrictions."
The code-red restrictions Manitoba enacted in November included some of the toughest measures imposed anywhere in Canada, even banningindoor socialization.
With the benefit of hindsight, Roussin suggested tough measures could have been imposed earlier in the fall, when the province attempted to contain the spread of COVID-19 with targeted restrictions, such as reducing the hours when Winnipeg bars could serve alcohol.
"In the second wave, the overall thought was take that incremental approach, try to target the epidemiology as much as you could," he said. Theapproach was successful in western Manitoba in August.
"We really wanted to rely on that going forward, but we quickly saw that the incremental approach and really trying to trying to limit the impact of those restrictions just didn't work when we started seeing more and more transmission."
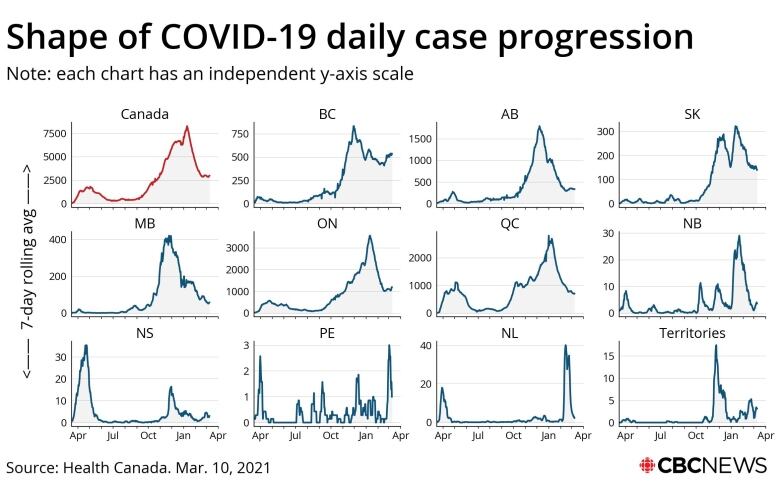
At the height of the second wave in late November and early December, the seven-day average daily case count topped out at 424.
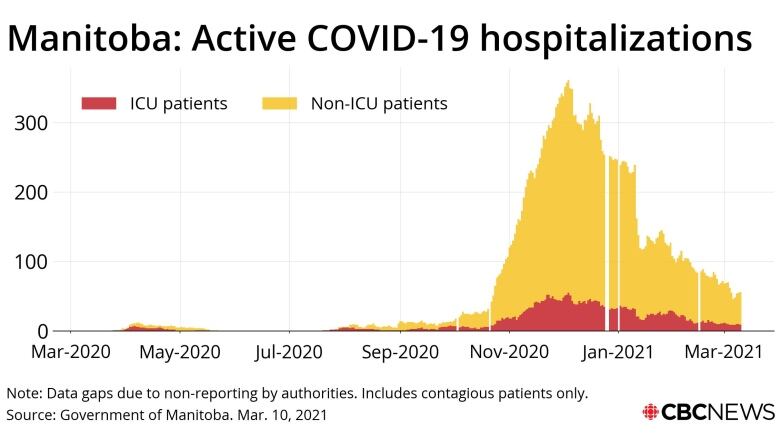
The number of COVID-19 patientsin Manitoba hospitals maxed out at 388. Intensive care units set up to serve 72 patients prior to the pandemic treated a high of 129.
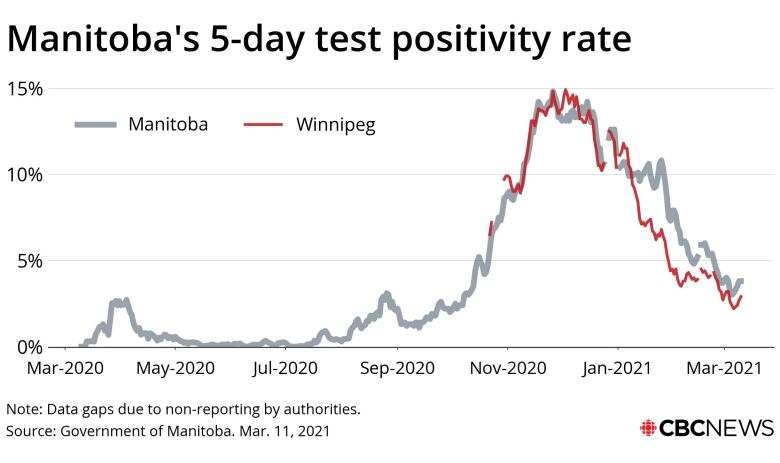
The COVID-19test-positivity rate capped out at 15 per cent.
Dozens of personal-care homes suffered outbreaks. As many as 19 COVIDdeaths were announced in a single day.
Manitobans were dying at a rate unseen anywhere else in Canada during the second wave, particularly in personal care homes.
This had yet to dawn on elected officials.
"There is no jurisdiction in Canada in which there have not been deaths in personal care homes. It is tragic, it is regrettable, but it is unavoidable," then Health Minister Cameron Friesen said in October.
Friesen's successor, Heather Stefanson, said in a statement the province is committed to preventing similar deaths in future pandemics, partly by implementing every recommendation flowing from the review of the outbreak at Maples Long Term Care Home, where 56 residents died.
"Certainly, we've learned a lot about this virus and how to bend the curve, and those lessons will be a valuable guide in future pandemics," Stefanson said in a statement.
The Progressive Conservative government had no pandemic playbook to follow, she said.
"Our government and public health officials have consistently made decisions based on the best available evidence, and have adapted strategies based on rapidly evolving information," she said.
Opposition Leader Wab Kinew, a New Democrat, said the government could have learned more from the first wave in other provinces.
"We had seen the terrible impact on the long-term care homes in Ontario and Quebec. We knew that there was a risk of community transmission ramping up early in the fall, yet the early warning signs were ignored," Kinewsaid.
"We see the impact in terms of how many people died in Manitoba. I don't need to resort to hyperbole because the facts themselves are so damning."
As Manitoba enters the second year of the pandemic, every indicator appears more positive.
Daily case counts are in the dozens instead of hundreds. The number of COVID patients in hospitals is less than half the tally at the peak during the fall.
COVID-19 test-positivity rates arein the low single digits. The daily death toll is measured in ones or twos.
Pandemic restrictions continue to ease every three weeks.
Most promising of all, complaints about a lack of testing and tracing resources have been replaced with complaints about the rollout of vaccination programs.
Even the most concerning new developments have proven to be less dire than initially feared, at least so far.
Outbreaks in remote Indigenous communities this winter have not resulted in the death rates seen in the Winnipeg health region in fall. The province has yet to detect manycases of more contagious coronavirus variants of concern.
Should a third wave emerge as a result of the variants, Roussin suggested Manitoba won't hesitate to impose a tough lockdown.
"I think that's something we'd have to consider earlier on," he said.












_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)



























































































