57 Health Accord recommendations include basic income, integration of services for N.L.
Details about implementation coming in the next 2 months, say co-chairs

The Newfoundland and Labrador Health Accord's long-awaited final reportmakes 57 recommendations to improve health outcomes and save money over the next decade.
Recommendationsinclude implementing a universal basic income, integrating ambulance services, reducing the number of emergency care centres and focusing more on the social determinants of health.
"We all know the health-care system needs to change, as we continue to spend the most per capita yet have the worst outcomes," said Premier Andrew Furey in a statement. "I look forward to reviewing this reimagining of our health-care system to take place over the next 10 years."
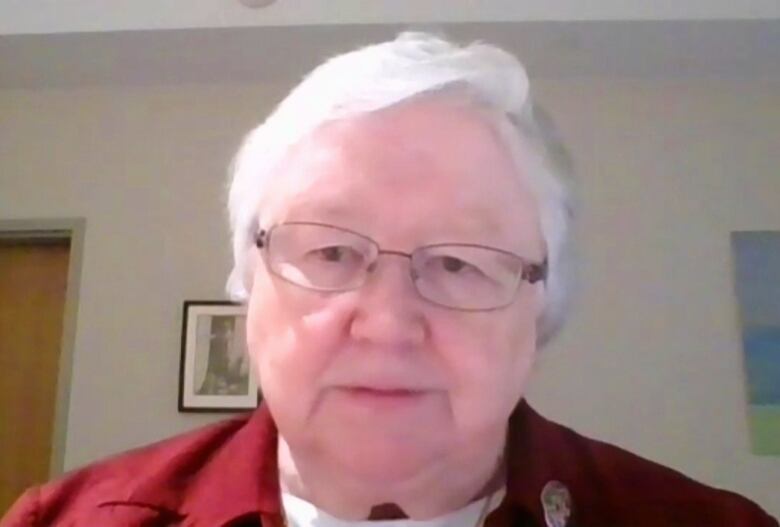
The Newfoundland and Labrador government created the Health Accordin November 2020, and tasked co-chairsSister Elizabeth Davis and Dr. Patrick Parfrey to evaluate problems in the province's health-care systems and develop solutions.
The report notes that people in Newfoundland and Labrador have markedly worse health outcomes than the rest of the Canadian population by most indicators. Newfoundland and Labrador's life expectancy is 2.4 years lower in men and 2.3 years lower in women thanthe Canadian average statistics that havesteadily worsened since 1980.
According to the report, the rate of children with complex health needs in Newfoundland and Labrador is 53 per cent higher than the national average, and the rate of chronic disease is worse too.
Though the report includes 57 calls to action and many more smaller recommendations, it does not delve into the cost of those measures. The authors say another report, called The Blueprint, will be released within two months and will show how the Health Accordcan be implemented.
Centralizing emergency services
Despite the province's fiscal situation, the report is light on cuts to health care though it does recommend finding efficiencies.
"We are not recommending taking any services out of any areas," said Parfreyin an interview with CBC News. "We need to plan for the realities that we're faced with."
The province's air ambulance service and 60 ambulance operators would be brought under one system with public oversight. There would be one central dispatch system for the province, and virtual care for rural areas. The plan also includes a separate transportation system for non-emergencies, which would free up ambulances.
"We have to have a system that works together," said Davis. She said the Health Accord task force has not determined whether the new system will mean cutting ties with any of the province's private ambulance services.
Additionally, emergency services at23 health centres serving fewer than 5,000 people would instead be provided by one of 13 hospitals less than 90 minutes away. The 23 health centres would still provide 12-hour urgent care, and would develop "collaborative-care models" that use virtual care to link to hospital emergency departments.
Parfrey said implementation would involve discussions with communities that will be affected.
The social determinants of health
The report focuses on the social determinants of health, or the social, economic and environmental factors that affect how people live. The authors argue that by improving those factors, the government can improve health outcomes too, and ultimately spend less on health care overall.
According to the report, the government of Newfoundland and Labrador has increased health-care spending by 232 per cent, but has increased spending on social programs other than education by just six per cent.
One of the most significant calls to action in the report is the implementation of a basic income at the federal level. The report does not specifically say what form that income should take, but says it should be targeted either at households living in poverty or for individuals below the poverty line.
"We believe that in the longer term, the best way to address poverty, the best wayto move people out of poverty and the best way to move people away from the indignity that comes from being poor is through a basic livable income," says the report.
Addressing an aging population
The population of Newfoundland and Labrador is aging, and the report has several recommendations for improving health outcomes for seniors, including the development of a formal frail elderly program.
The report says N.L. emergency departments are not "senior-friendly," with seniors often being treated for a single problem, rather than for other health issues that may have led to the visit.
A formal frail elderly program would ensure that seniors receive care for multiple health concerns at once, reducing the potential for readmission, according to the report.
The report calls on the government to develop legislation that will support the rights of seniors in the areas of health and housing, including in long-term and personal-care homes.
Community care teams
The report addressed the harm caused by physician and nursing shortages across the province. According to numbers from the Newfoundland and Labrador Medical Association, nearly 100,000 residents don't have a family doctor.
"Such high turnover and vacancy rates cause significant challenges for continuity of care for patients/clients/residents, for sustainability of specific programs, and for stability within the health care communities," said the report.
The report recommends establishing 35 new "community teams" that will include family physicians, nurse practitioners, pharmacists andsocial workers. The teams would serve a population base of 7,000 residents or more, and, according to the report, would ensure more timely access and continuity of care for more people.
Newfoundland and Labrador's net debt was $16.7 billion as of November, and any changes to the health-care system will have to be done within the province's fiscal constraints.
However, according to the report, the Health Accord was not specifically tasked with saving money.
"Over the longer term, health transformation will help improve health outcomes a healthier population will place fewer demands on the health system," the authors said.
With files from Carolyn Stokes












_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)