Death count rises as N.L. grapples with painkiller addictions
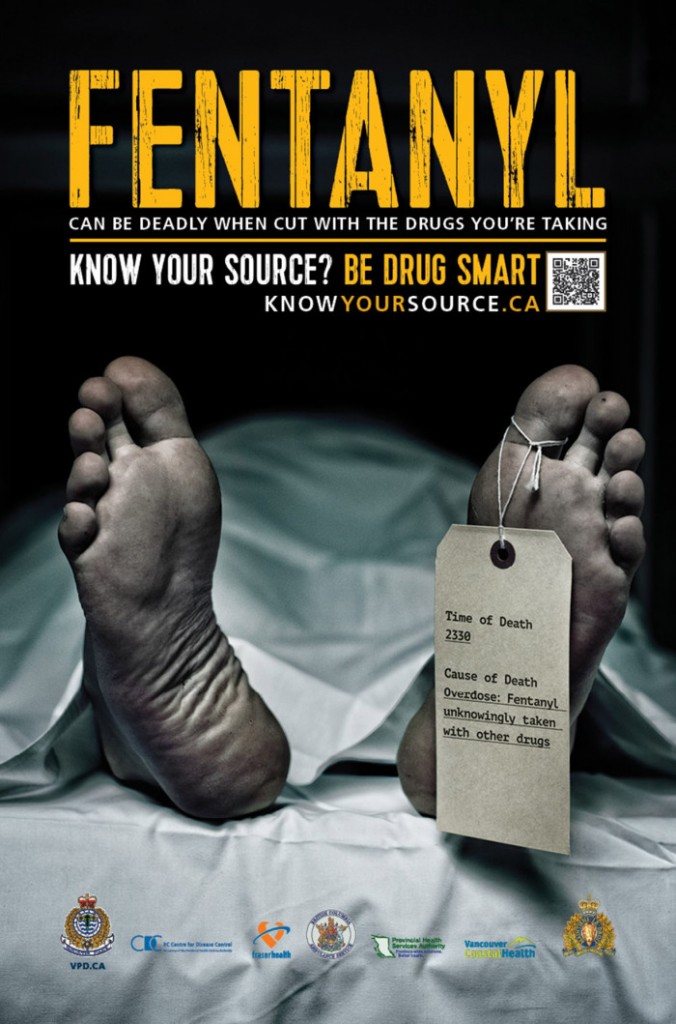
'When drugs are mixed with [illicit] fentanyl it's lethal and people don't know what they're taking'

In 2017, health authorities called together the media to make a public warning fentanylwas in Newfoundland and Labrador, and was suspected in a string of overdoses within a two-week period.
Last year,23 people died of opioidoverdoses and 57 people were hospitalized, according to figures provided from Dr. Simon Avis, the province's chief medical examiner, to police.
"There's a significant increase inoverdoses," Royal Newfoundland Constabulary Sgt. Steve Knight said in a wide-ranging panel discussion on the St. John's Morning ShowTuesday.
He added the overdoses were related to a number of opioids, including OxyContin, morphine, fentanyl, carfentanil, and hydromorphone.
In 2015, there were 20 overdose deaths province-wide.
Hard to pinpoint all overdoses
CBC News asked for the 2017 numbers broken down by region and by drug through access to information requests, but wastold the data has not yetbeen completed.
However, the official number of people who overdosed and survived is likely skewed.
"They're using the naloxone kit and forget the next bit, which is to call 911," said Newfoundland and Labrador's Health Minister John Haggie, who is also a surgeon.
"We don't know howmany those are."
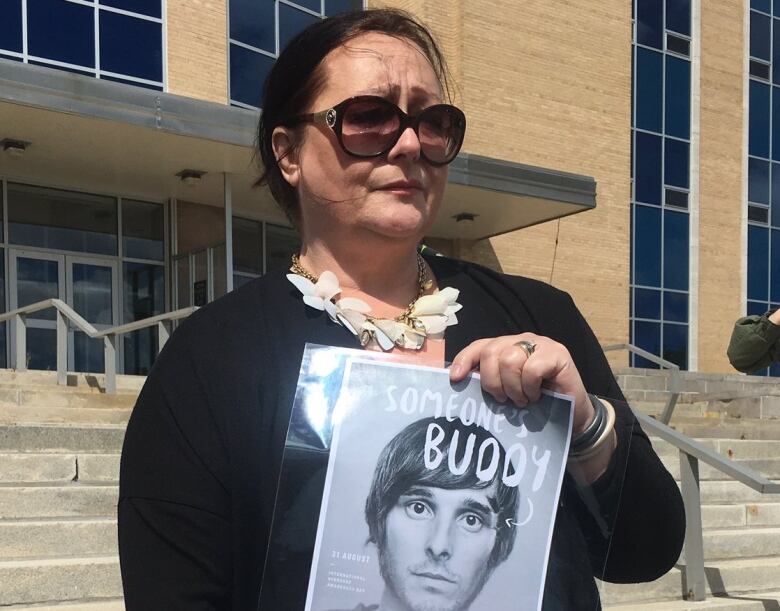
Tree Walsh has abettersense of the truth behind the statistics, having worked as an advocate for years.
She did a line of coke, man, she didn't think she was going to die.- Tree Walsh
Walshdistributes clean needles and naloxone kits which can reverse an opioid overdose as part of the Safe Works Access Program (SWAP).
"It sounds like it's happening quite frequently," she said. "People are reluctant to talk about the situation."
Walsh said she is hearing from drug users that the two vials of the antidote that comes in a typical naloxone kit aren't always enough to match the strength of the drugs on the street, and users have to give multiple doses in order to reverse the overdose.
Cocaine, heroin 'bigger drugs' in N.L.
From a policing standpoint, Knight said officers are noticing many prescription medications that are being abused on the street as well as other drugs that weren't as common years ago.
"Cocaine is probably one of the bigger drugs in our province right now, and we are starting to see an increase in heroin use," he said.
Those drugs are being cut with illicit fentanyl that's coming from the west coast of the country, he said.

"When drugs are mixed with this fentanyl it's lethal and people don't know what they're taking," Knight said, who works for thethe Combined Forces Special Enforcement Unit.
Walsh, through her work with SWAP, is also hearing stories of street drugs being mixed with fentanyl as a way to improve dealer's profit margins.
She recounted hearingfrom friends about awoman who died over Christmas.
"She did a line of coke, man, she didn't think she was going to die."
Not quite a crisis
Despite the increase in overdose deaths, Walsh stopped short of calling it a crisis but rather a personal crisis for those who are living it.
Haggie, meanwhile, points to the government's efforts to educate doctors on prescribing opioids.
"There's enough prescription opioidsprescribed to give every man, woman and child a twice week course of opioids each year," Haggie said.
"Addictions startwith a pad as far as we're concerned."
A new program launched last November aims to flag health professionals ifa person has visited multiple doctors in an attempt to get drugs.
ButWalsh is hearing from pain patients who began injecting their prescription when the drugs no longer meet the need, and fear what will happen if they're cut off from their prescription.
"They're terrified. They're afraid thattheirdoctor will be put under scrutiny forprescribingtoomuchopioids," she said.
She said one manwho uses SWAP fears he will have to go to the street for his drugs if that happens.
Introducing Suboxone
In 2016, Haggie and his department introduced an alternative to methadone treatment.
Suboxoneis less prone to cause an overdose because of its chemical composition, and can be taken in a tablet form, instead of as a liquid like methadone.
"They don't have to line up at the drug store at 8 a.m. in the morning to get theirdose," Haggie said,comparing it to methadone.
Numbers obtained by CBCNews show far more individuals are on methadone than its reported safer alternative, Suboxone.
Between May 26, 2017 and Dec. 31, 2017, the health department said 1,954 people had prescriptions for methadone. It came at a cost of$2,990,931.66 to the Newfoundland and Labrador Prescription Drug Program (NLPDP).
Within that time frame,376 people had prescriptions for Suboxone. Those prescriptions cost $153,626.87 to the NLPDP.
With files from the St. John's Morning Show












_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)