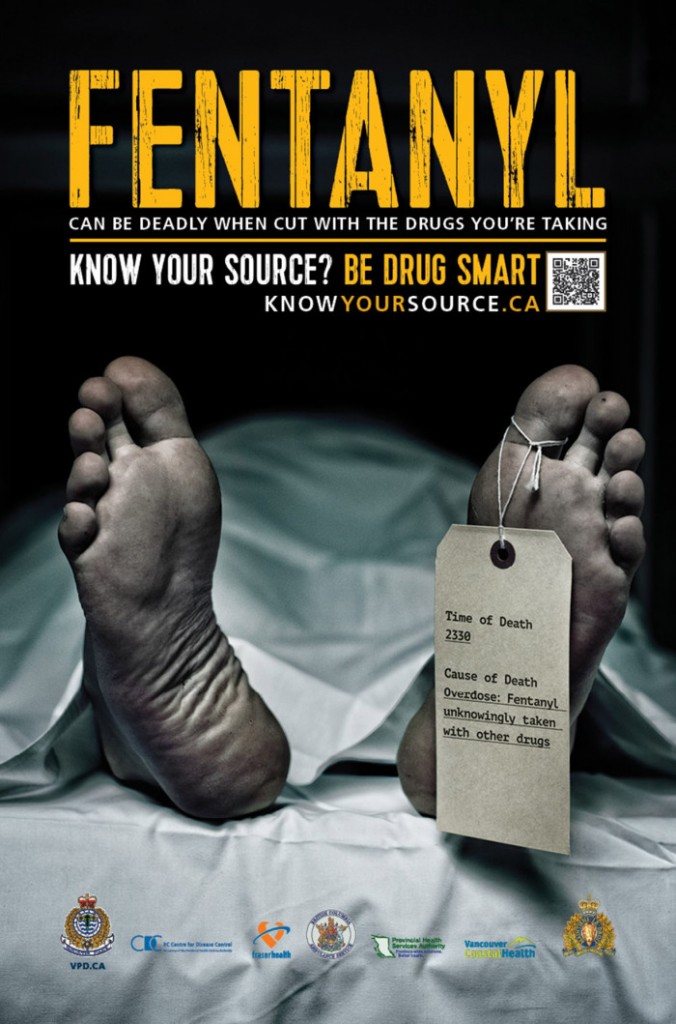
Better monitoring of painkiller prescriptions needed, says Yukon coroner
2 patients died of mixed drug toxicity in 2012 after obtaining large quantities of drugs

Yukon's Chief Coroner is calling for a territory-wide system where doctors and pharmacists can share information on patients' prescriptions after investigating two deaths from mixed drug toxicity.
In both cases, coroner Kirsten Macdonald found that the patients had obtained large quantities of prescription painkillers, either by refilling prescriptions early or visiting multiple clinics and pharmacies.
While the deaths both happened in 2012, the coroner's reports were only published a month ago. The Chief Coroner notes a three-year wait is "atypical in the amount of time" for an investigation.
'A history of multi-doctoring'
Francis Caouette died in July 2012 at a campground in Faro. An autopsy showed he had elevated blood levels of an opioid painkiller and multiple other medications were found in his system. He was found to have died of mixed drug toxicity.
Macdonald's report says the 35-year-old man had "a history of multi-doctoring," visiting multiple clinics for prescriptions and getting them filled at multiple pharmacies.
"He exhibited drug-seeking behaviour by requesting an increase in the dose of medication and for prescriptions to be filled early. Mr.Caouette would rotate the pharmacy every time he filled a prescription to avoid early detection of early refills of narcotic medications," says the report.
In April 2011 and March 2012 Caouette was hospitalized for "deliberate overdoses of prescriptions medications."

"The only way for a family physician in Yukon to confirm all the prescriptions written and dispensed for his/her patient is to call each of the pharmacies and request the information," Macdonald notes in the report.
She says the inability of pharmacies to review whatCaouette had previously been prescribed and dispensed allowed him to obtain large quantities of medicationwithout detection.
'Large quantities' dispensed
The second case is that of Judith Foster, 63, who died in September 2012 in Whitehorse. Foster had chronic pain due to a motor vehicle accident and a back problem.
She was being prescribed two opioid painkillers along with other drugs that can cause drowsiness and was allowed to "self-adjust" her dosage for some medications. Foster also had a history of prescription medication overuse and past illicit drug use.
"At the request of Ms. Foster, multiple early renewals in large quantities of medication were prescribed and dispensed," Macdonald writes.
The report says none of the screening or monitoring tools under the Canadian guidelines for prescribing opioids for chronic non-cancer pain were applied in Foster's case.
Coroner recommends action
Macdonald makes two recommendations. One is for Yukon's Department of Health and Social Services to create a prescription information system to allow doctors and pharmacies to share information on what medications have been dispensed to patients.
Her second recommendation is for the Yukon Medical Council to consider requiring doctors to send certainprescriptions directly to pharmacies instead of handing them to patients.
Yukon's territorial government is currently finalizing a new Pharmacy and Drug Act, which will modify regulations for community pharmacies and rural dispensaries.
Pat Living, who represents the Department of Health, says the territory is also working on digitizing health records. One component of that work is a drug information system.
"All the healthcare providers, whether it's a physician, a pharmacist, a community health nurse...they would be able to view a patient's medication profile," she says.
"It would be able to prevent some of this overmedication and people being able to go from one doctor to another."
Living says the system could launch within 18 months.












_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)