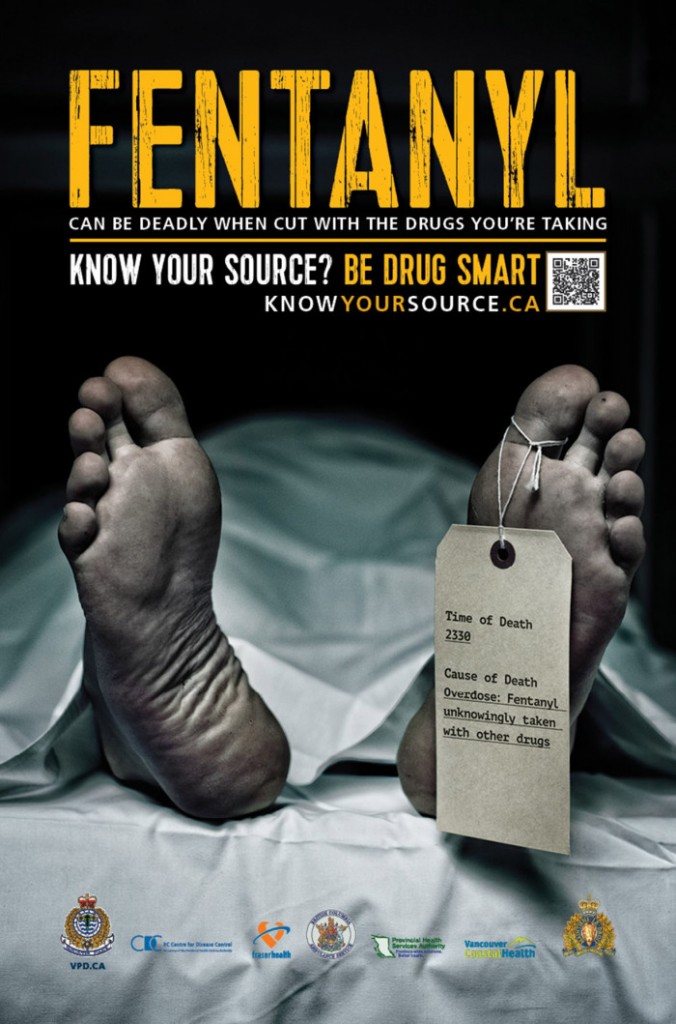
Prescriptions led to 1 in 3 opioid deaths in Ontario in 2016, study says
Illicit or bootleg fentanyl contributes to most opioid-related deaths in province

About a third of deaths caused by opioids in Ontario in 2016 were among people who had been prescribed the drugs, a study published Wednesday indicates.
It's a trend researchers expect will continue to decline but not disappear as the scourge of illicitly obtained fentanyl overdoses continues.
In the mid-1990s, Canadian doctors expanded their prescribing of opioidsto people with moderate-to-severe pain rather than only people with terminal cancer. Those drugs could be diverted by people sharing or giving away medication, as well as being stolen and then sold illicitly on the street.
As opioid-relateddeaths climb in North America, researchers and policy makers have been searching for information on the role of prescribed versus non-prescribed opioidsin the deaths.
- CBC INVESTIGATES | When prescription opioids run out, users look for the supply on the streets
- B.C. attorney general announces lawsuit against opioid makers for 'negligence and corruption'
The federal government says that as of June, a total of 3,987 apparent opioid-related deaths were reported in Canada in 2017. Of these, 92 per cent were accidental and mainly involved fentanyl or analogues such ascarfentanil.
In a study published in Wednesday's issue ot the British medical journal BMJ, researchers spell out the role of prescribed, diverted and illicit opioids to opioid-related deaths in Ontario.

They conducted the analysis by reviewing medical coroners' charts for all deaths determined to be opioid-related in Ontario from 2013 to 2016. The study's authors also reviewed billing records for physician services and information from the province's narcotic monitoring database for drugs sold at community pharmacies.
Among the 2,833 opioid-related deaths in the study, one third, or 997, were among people who had an active opioidprescription at the time of their death.
- SECOND OPINION | New questions about old Canadian study foreshadowing opioid crisis
- Opioid epidemic fuelled by 1 paragraph in journal, doctors say
"To me, given the conversation right now and how much of a focus there is on [illicit]fentanyl, I think some people might be surprised that one third of deaths still are occurring among people who are actively receiving prescription from their physician," saidstudy author Tara Gomes, a scientist at St. Michael's Hospital in Toronto.
Lethality of illicit market
For those who died without a prescription, the researchers still found a high degree of prescription opioids such as oxycodone, hydromorphone and methadone. The findinghighlights the role that diverted prescriptions play in fatal overdoses in the province, Gomes said.
Gomes strives to understand the interplay between prescribed and illicit opioids, given how doctors are now less inclined to prescribe the drugs. People may move to buy less safe versions on thestreet. She expects the contribution of prescription opioids to total deaths will decline.
Currently, illicit or bootleg fentanylcontributes to most opioid-related deaths, based on coroner's reports and toxicology tests. For Gomes, the mounting deaths and the blow to families hammers home the importance of taking a multifaceted approach that includes harm reduction.
"Unfortunately, everything that we've been trying so far has had limited impact," saidGomes, who is also a researcher at theInstitute for Clinical Evaluative Sciences.
Harm reduction has "been top of mind, with the changes in the provincial government recently [and] with the pause that has been put in place for supervised consumption sites and overdose prevention sites. But really, at this point, given the lethality of the illicit market, we really need to focus on providing people with safe places to use drugs to prevent them from dying if they do overdose."
She suggests three longer-term responses:
- Provide better, quicker access to treatment for people who've developed an opioid use disorder.
- Promote more appropriate prescribing so fewer people become dependent on and addicted to these drugs.
- Put in place policies to prevent large quantities of these drugs being dispensed from pharmacies, so thathuge amounts of these drugs aren't sitting in people's medicine cabinets or being made available for people to divert and sell to the illicit market.
The researchers also found just over 40 per cent of those who died had visited an emergency department for a mental health reason in the previous three years.
- Suboxone recognized as new first line of treatment for opioid substitution therapy
- The pill to manage addiction: why so few doctors are prescribing Suboxone
"For me, one thing that was the largest finding was that approximately half of the individuals wereseen in the last 180 days. So they were interacting with the health-care system in some manner andperhaps those are really missed opportunities to flag patients that are really high risk," said study co-author and pharmacist Mina Tadrousofthe Ontario Drug Policy Research Network.
"This points to giving tools to frontline health-care workers," to direct patients to non-pharmacological treatments for pain and addictiontherapies.
One option is expanding rapid access to methadone or Subxonein emergency departments, because those visits might be a time patients are open to discussing addiction treatment.
Gomes added more doctors need to be trained to offer it. Patients also need to be at a specific stage of withdrawal.
The study's authors said their findings on the proportion of deaths involving a prescription were comparable to those reported in British Columbia and Alberta.
With files from CBC's Amina Zafar












_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)