The dementia tsunami is coming, fast . We all know it, and it will affect every single one of us, either directly or through our loved ones. That we are not prepared for such an onslaught is an understatement. Dementia is an expensive disease, and if we do the maths, we can see that our current health care system and long-term care infrastructure cannot hold up to what is to come.
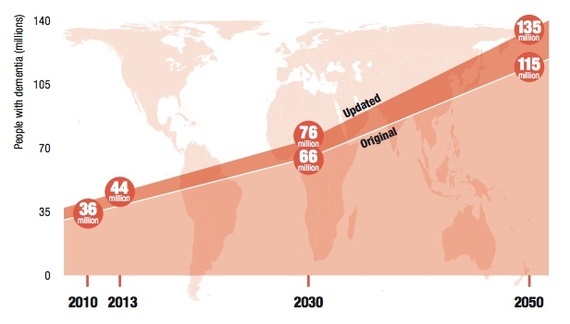
(Chart from The Global Impact of Dementia 2013-2050 )
The dementia problem requires high level solutions from multiple sectors: public health, health care, community, business, and technology. It will take a whole world to effectively tackle the problem. Those solutions need to be thought out from the ground up, starting with the persons with the disease and those caring for them. As someone working in the trenches of dementia, here are some no-nonsense strategies to help mitigate the problem:
1. Better prevention
The current consensus leans towards the need to emphasize a whole suite of lifestyle and diet factors. According to a National Institute on Aging report and the Alzheimer's Association , here are six things you can do to promote brain health:
- Do 30 minutes of aerobic exercise every day. Exercise is good for the brain and also helps decrease cardiovascular risk factors, a known risk for dementia.
- Maintain a healthy diet rich in fruit and vegetables. Like exercise, eating healthy can help with cardiovascular factors. It also helps with obesity and diabetes, two other major risk factors for dementia.
- Remain socially active. Keep on working, volunteer, join social clubs, travels, get out.
- Engage in intellectually stimulating activities. Exercise your brain by doing crossword puzzles, taking courses, playing social games, reading, writing, gardening...
Most remarkable is the fact that exercise, diet, socialization, and mental stimulation combined have been shown to be more likely to lower the risk of dementia than any one of those factors alone! This information needs to be broadcasted more broadly to overcome the amount of misinformation in the general public.
2. Better diagnosing
For a disease category that is bigger than either heart disease or cancer alone , dementia is being treated like the poor cousin of illnesses by the medical field. This is due in part to the prevalent attitude that no cure means no hope. The truth is this not the case, and getting a proper diagnosis early on can make a big difference in the quality of life for both patients and their families. It also has the potential of saving big money to large institutions such as Medicare and other health insurance companies. Right now, the most likely scenario is for the patient to receive a generic dementia diagnosis from a primary care physician after a quick evaluation. This is ignoring the fact that dementia is not a disease, but rather a cluster of different dementia subtypes, each with a different etiology, prognosis, treatment, and behavioral manifestations. Here are several reasons why an accurate diagnosis is important:
- A mild cognitive impairment diagnosis can motivate patients to make lifestyle changes, with the hope that those might delay a progression to full-blown dementia.
A better understanding of dementia and of the best places to get an accurate diagnosis need to be provided to both the general public and to health care professionals. Neurologists and memory care clinics should be the go-to places for an accurate dementia diagnosis.
3. Better caregiver support
Statistics from the Alzheimer's Association speak to the extraordinary stress suffered by dementia caregivers, with 40 percent suffering from depression and 72 percent expressing relief when their loved one dies. This is due to the unique challenges from the illness in terms of its intensity, duration, unpredictability, and all encompassing features. Caring for a loved one with dementia is akin to running a marathon one did not sign up for, and more importantly one did not prepare for. Such care burden demands that caregivers be supported in ways that can sustain them throughout the duration of the disease:
- The Mindfulness-based dementia care (MBDC) training can help with lowering caregiver stress while at the same time promoting an enduring sense of self-efficacy in their caregiving interactions.
4. Better residential options
When comes the time for the person to move into an assisted living community or a nursing home, affordable and quality options are few, if not impossible to find. This is due in part to the high labor costs associated with high quality dementia care, along with stifling regulations, and a lack of innovation from the assisted living industry. The big question we all need to ask ourselves is, would I want to move into any of the current living alternatives offered to persons with dementia? If the answer is no, we know something has to change. The way of the future for residential dementia care might look like this:
- We can create dementia villages such as the one in the Netherlands where residents can continue to function in ways that maximize their sense of well-being. Dementia does not change our basic needs to come and go as we please, to continue with our pre-dementia routines of work and home life, and to be part of a larger community.
None of these solutions are impossible. Some can be implemented relatively easily and quickly. Others will require more coordinated efforts, and greater investments. All demand that we move from a place of denial and fear, to one of hope, creativity, compassion and action. It is not all downhill from the time of diagnosis, but rather an opportunity to create new ways of being with each other, within our families, and the larger community. We want to do this for ourselves, and also our loved ones.
Disclosure: The author of this post is the founder of the Presence Care Project , a non-profit organization with the mission to share and research the Mindfulness-Based Dementia Care program.












_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)



























































































