Fentanyl antidote kits from Alberta non-profits saving lives
119 drug users in central Alberta got a second chance at life thanks to naxolone kits
A program to distribute take-home naxolone kits to drug users has prevented119 deathsin central Alberta overthe last year.
Turning Point, an agency in Red Deer, started distributing naloxonekits in July 2015. Since then, the kits have given119 people a second chance at life.
"It dramatically proves that the program is effective and that it's needed," said Jennifer Vanderschaeghe, the executive director of Turning Point.
"Our number of reversals in central Alberta is larger than the rest of the province combined from our peer organizations."
The Take HomeNaloxoneprogram is making theantidote to fentanylavailable through Turning Point and other non-profit community agencies around the province.
Alberta Health beganfunding the programthrough an initial $300,000 grant in April 2015.
'They trust us'
Turning Point was the first agency to start handing out naxolone. In the last year,staff have distributedabout 500 kits andtrained people how to use them.
While naloxone kits are now available without aprescriptionat pharmacies in Alberta, Vanderschaeghe said it's critical for agencies that work with drug users to be able to hand them out as well.
"We have 17 years of working with people who use drugs. That means we have a lot of relationships with people who are already using opiates and they trust us," she said,adding the agency distributes43,000 cleanneedles to about 600 people each month.
Turning Point is one of sevenagencies distributing the kits in eight communities.

Vanderschaeghe said it's impossible to know how many of the 119 users the kits have saved were overdosing from fentanyl. She saidsome could have been using other opiatesora combination of drugs.
But fentanyl, which is considered to be approximately 100 times more potentthan heroin or morphine, has become a leading drug of choice on the street. In2015,fentanyl killed 274 Albertans.
The fact take-home kits prevented119 deathsis significant but the total the number may be higher.
Other people who survived an overdose by using the kits may have neglected to tellthe agencyabout it.
Alberta government pleased with results
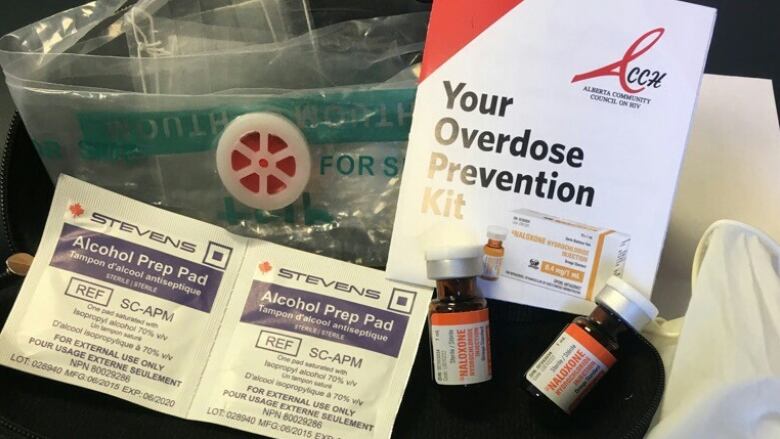
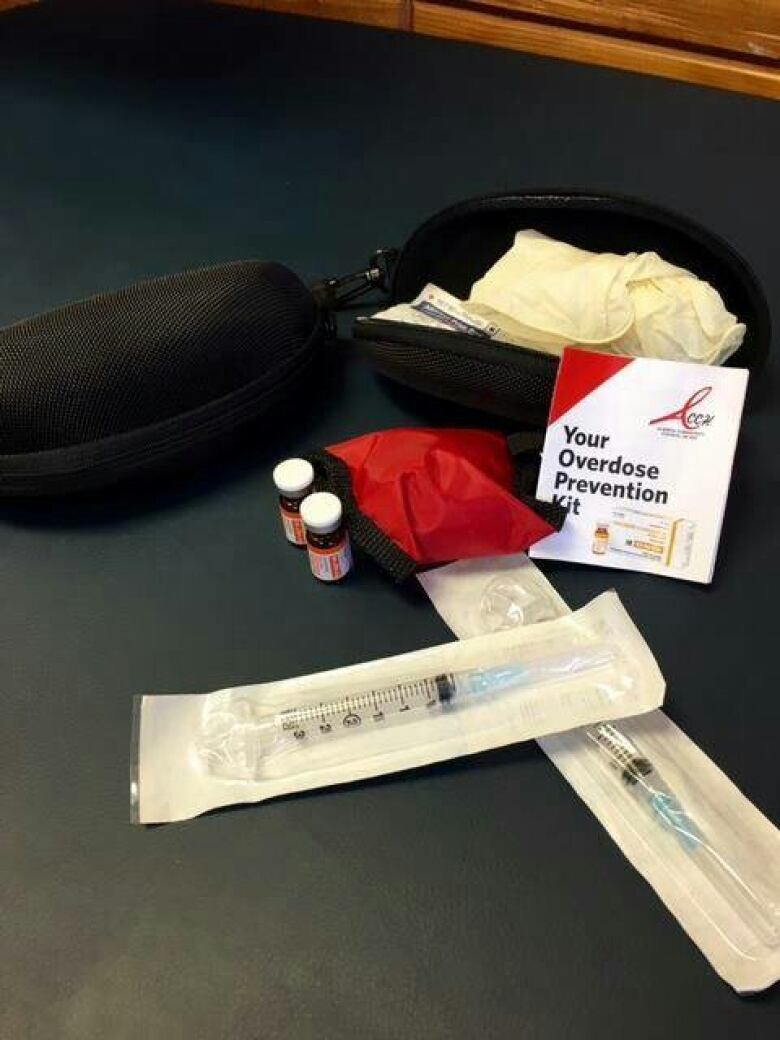
The kits contain everything needed for twodoses of the antidote:two vials of naloxone, two needles, two alcohol swabs and a pair of latex gloves.
Since people who have overdosed are unconscious,Vanderschaeghe saidthe injections are normally done by a friend or family member of a drug user.
The program Streetworks in Edmonton was the first agency in the country to hand out naloxone kits in 2005. Staff knowof 42 people who used them in the last year.
"We're incredibly pleased with the impacts we've been able to see through some of our community agencies," said Brandy Payne, Alberta's associate minister of health.
"Front-line agencies have been working side-by-side with the government since our naloxone program started," said Payne.
About 9,000 naloxone kits have been made available at 800 locations acrossthe province such as pharmacies andwalk-in clinics.
Payne isn't ruling out additional funds foragencies who believe they can make more of a difference if they can hire more staff.
Jennifer Vanderschaeghefrom Turning Pointsaid the $21.50cost of a naloxone kit is a small price to pay for the difference it can make.
"We're really looking at 119 people who had another opportunity to live, had another opportunity to look at making changes," she said.












_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)



























































































