Cervical cancer could be eliminated in N.B. in about a decade, says provincial oncologist
Outreach to underserved communities, vaccine promotion keys to success, says Cancer Society
The rate of cervical cancer in New Brunswick is either holding steady or increasing slightly, depending on who you ask, but the head doctor with the New Brunswick Cancer Network and the Canadian Cancer Society both agree the disease could realistically be wiped out in little more than a decade.
The Canadian Cancer Society's latest annual statistical report showed the national cervical cancer rate has begun to increase significantly.
Following a 30-year decline, incidence has risen 3.7 per cent a year since 2015, representing the biggest jump for any type of cancer affecting females.
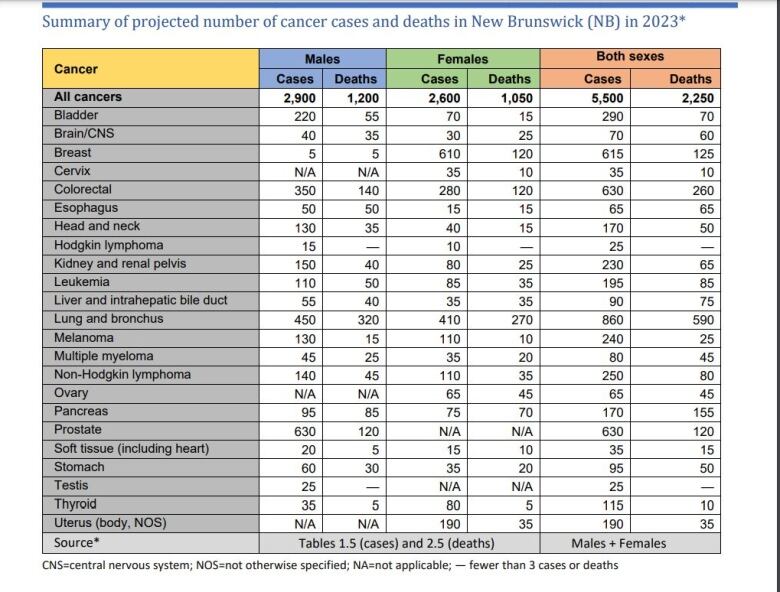
The latest projections for New Brunswick are 35 new cases a year and 10 deaths.
Dr. Eshwar Kumar of the New Brunswick Cancer Network said that's on par with the average number of new cases for the past 15 to 20 years.
If you look at some other statistics, however, New Brunswick is seeing a slight increase, said Heather Mulligan, manager of advocacy for the Canadian Cancer Society in Atlantic Canada.
For example, the age-adjusted rate per 100,000 females in the province is now 8.8 new cases a year, she said, up from 7.5 two years ago.
In 2021, cervical cancer was estimated to account for 1.2 per cent of all new female cancer cases in the province, she said, but the 2023 estimate creeped up to 1.3 per cent.
A variety of factors could be behind the increase, such as demographics, said Mulligan.
The human papilloma virus vaccine only came out in the 2000s, she noted.
It's now known that HPV, a sexually transmitted infection, causes virtually all cervical cancer, said Mulligan. (According to the Cancer Society, HPV is also linked to cancers of the penis, anus, vulva, vagina, mouth and throat.)
"The things that we have in place will hopefully reduce the risk considerably and hopefully eliminate it," said Kumar.
New Brunswick has a well-established HPV vaccination program. Immunization clinics are held in schools for all students in Grade 7.
Any females born since 1995 and males born since 2005 who missed getting the shot in school are still able to get it for free until the age of 27.
Outside of those birth dates and age ranges, anyone who wants the shot must get a prescription and pay for it.
The target is to get 90 per cent of 15-year-old girls around the world vaccinated by 2040, said Kumar. Canada expects to achieve that goal by 2030 or 2035 at the latest, he said.
The most recent vaccination figures in New Brunswick are headed in the wrong direction.
According to a provincial Health Department report on school immunization, the female participation rate in the Grade 7 vaccine program fell to 75.5 per cent last year, down from 81.5 per cent the year before.
Kumar acknowledged there is room for improvement.
In order to avoid getting vaccinated, some children don't go to school on the day clinics are held, he said.
Sensitive issuein some cultures
The participation rate in screening is also lower than he would like, he said, particularly in some cultural communities.
"I think there's been a lot of immigration from countries where perhaps things like this screening for women is culturally sensitive," said Kumar.
That may be partly because HPV is sexually transmitted, he said.
In "many, many" cultural communities, preventive health care for women is "probably not as strong as it can be," said Kumar.

He is optimistic that a bit of outreach can make a big difference.
"Many of our staff are actively involved, going out to the community, meeting with newcomers and trying to get them to understand why it's so important and what we can achieve by participating."
Cervical cancer screening has been promoted very proactively, said Kumar.
"In spite of the fact that sometimes we may be short of resources, we have not hesitated to promote screening as being an important aspect of reducing the burden of cancer."
The health authorities have been "very, very good" at opening up clinics for pap testing, he said, estimating there are about 20 around the province, available to women who don't have a family doctor.
Women aged 21 to 69 are eligible.
Research is underway at the universities to identify barriers for various communities of new immigrants, he added, then education and awareness activities will be tailored to try to address those concerns.
The ability to take a screening test in one's own home will also be a "huge step forward," said Kumar.
That's supposed to start within the next five to seven years, as the province transitions from pap testing to HPV testing.
The phased-in plan is for primary HPV testing to commence over the next 12 months, while pap smears continue to be done, said Kumar.
An advisory committee of primary care physicians, nurse practitioners, gynecologists, lab directors, pathologists and oncologists is currently working out what will be New Brunswick's standards for HPV testing, including the frequency required, method of testing, interpretation of samples and guidelines for clinical practices and reporting.
"We need to ensure that the lab infrastructure is in place and the lab standardization has occurred. That's going to take us about a year."
Computer systems also need an upgrade, said Kumar, to keep track of HPV testing and ensure followup care for patients.

The Cancer Society is "thrilled" that PEI and New Brunswick are "leading the charge," in terms of transitioning to HPV testing, said Mulligan, while adding that more needs to be done.
At-home testing is really important, she agreed, as well as identifying underserved and undervaccinated populations.
"Every effort should be taken," said Mulligan.
"We have an opportunity in front of us to say we live in a province where cervical cancer rates are low or non-existent."
For so many other cancers, the risk factors and deaths are many, while effective preventions and treatments are few.
A cancer with different outlook overall
According to the statistics, there are about 20 kinds of cancers that affect and kill more people. At the top of the list are lung, breast, colorectal and prostate.
When it comes to cervical cancer, "it's a matter of vaccination, treating infection and preventing spread," she said. "We can get it off the list."
National and international goals have been set to eliminate cervical cancer by 2035 or 2040.
"It's very rare very unusual for oncologists and people involved in cancer to talk about eliminating cancer," said Kumar.
"I've been an oncologist for quite a long time now and I still am excited about the possibilities of the things that we can achieve," he said.













_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)