COVID-19 in Sask: Who gets a ventilator? In 'hypothetical' worst-case scenario, age might decide
Sask. reports 14 new cases including assisted-living care centre worker in Regina

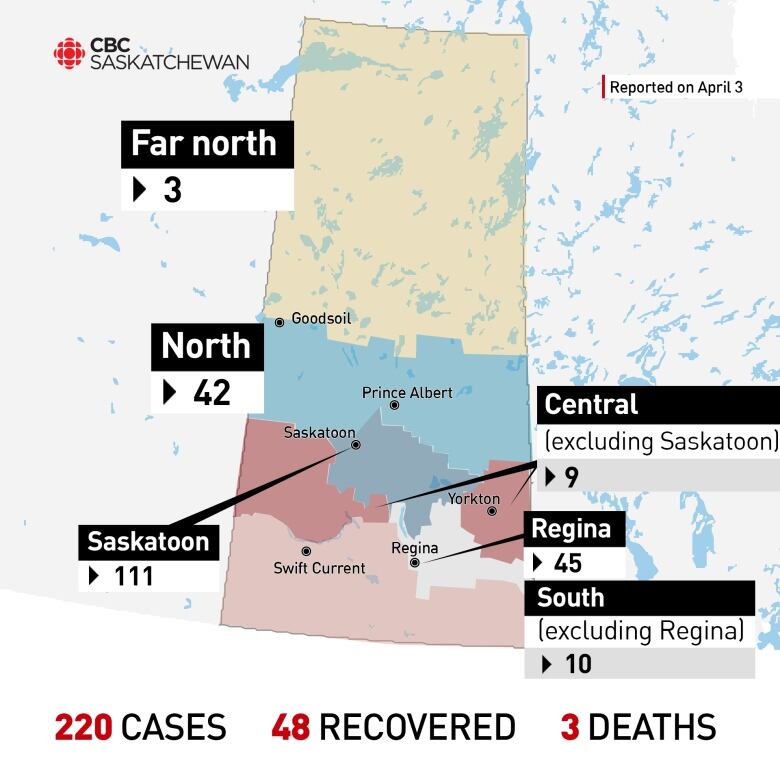
- Saskatchewan reported 14 new cases of COVID-19 Friday, bringing its total to 220.
- Forty-eight people have recovered from the virus in the province, making for a recovery rate of 22 per cent of known cases.
- An assisted-living care centre worker in Regina has tested positive for the virus.
- A long list of professionals has petitioned the province to release inmates in light of the pandemic.
- Saskatchewan's privacy commissioner says "more information is better'" during a health crisis like COVID-19.
The Saskatchewan Health Authority has offered an early glimpse at some ofthe factors health care teams might weigh to decide which COVID-19 patients get ventilators if there are not enough to go around.
Dr. Susan Shaw, the SHA's chief medical officer, said the details are still being finalized and, at the moment, remainhypothetical.
"We're not there right now," Shaw said in an interview Thursday.
While it's not clear, cumulatively, how many of Saskatchewan's COVID-19 cases have needed a ventilator, the maximum number of coronavirus cases who have been under intensive care (ICU) at the same time is known to be two.
As of Thursday, four COVID-19 patients were in hospital in the province, including two people in ICU.
Shaw's colleague Dr. Saqib Shahab Saskatchewan's chief medical health officerand the public face of the province's fight to "flatten the curve" said it's hard to know when the province might reach its infection peak.
"Obviously at some point we want to see the curve going down. Is that going to be in four weeks, eight weeks? We really can't predict," he said on Wednesday.
The province currently has 450 ventilators and has ordered hundreds more. One early-draft planning doc, leaked last week, estimated thatat peak infection time, Saskatoon alone might need 500 to 600 ventilators at a time.
Health officials in Saskatchewan and elsewhere have undertaken the grim but necessary exercise of contemplating who would get a ventilator should hospitals be swarmed with serious cases while not having enough machines to go around.
"One of the main purposes of actually having this work done in preparation is a part of our responsibility to avoid arbitrary decisions," Shaw said.
"Right now the decisions are made about what's best for the individual. And when you get into a situation where you're starting to actually face scarcity, the ethical principles shift to be what's best for society."

Age is not the only factor
Decisions about which patients would get ventilators would be made by doctors and members of the health authority's ethics commities, Shaw said.
The age of patients is a key consideration, but not the only one, she said.
"It's actually one of a combination of criteria," she said. "To make decisions solely on age would be discriminatory and would not be the way we would want to approach this. It's age in combination with frailty, chronic disease and recoverability."
In the "extremely unlikely" scenario where two patients' criteria lined up exactly, the ventilator would go to the younger patient, Shaw said.
"That's based on the principle called the goal of the life cycle, which is every individual needs to have the equal opportunity to live through the various phases of life."
-
At the Top of the Covid-19 Curve, How Do Hospitals Decide Who Gets Treatment?
-
What is a ventilator and who gets one if COVID-19 turns catastrophic in Canada?
No one would completely stop being cared for, however.
"That always applies no matter what the situation is," Shaw said. "This means making sure that we never abandon the patient."
Medical health professionals elsewhere have also contemplated the notion of a lottery.
While Shaw stressed that that option is not in Saskatchewan's current way of thinking, she is familiar with the concept.
"My understanding is that if you ever got into a tiebreaker situation where absolutely everything [including age] was identical and again I think this is absolutely hypothetical then a lottery is one of the ways that you could tackle that."
New numbers,Regina worker tests positive
Friday's daily update from health officials included 14 new cases, bringing the total provincial tally to 220.
Shahab said the comparatively low daily case additionsin Saskatchewan which have averaged 14 per day, after the province saw its largest day-over-day increase of 30on March 27 "are to some extent reassuring."
"However, we are seeing that less and less of those are due to travel," he said.
Of the total 220 cases, 102 are recent travellers, 52 tested positive because of exposure to someone they live with or after they attended an event, 10 have no known exposuresand 56 are still investigation.
The province added yet more detail to its daily report, for the first time specifying what region each fatal victim of the virus came from.
Shahab was asked about specifying which community an infected person came from (beyond Saskatoon and Regina).
"As our numbers increase that becomes easier to do," he said.
Here's how the cases break down regionally.
The province said a worker at Eden Care, an assisted living facility in Regina, has tested positive for the virus. The person was identified by another positive test case, through the process known as contact tracing.
"There are no indications it has spread to other employees or residents," the health ministry said in a release. "The facility is closed to admissions, discharges and transfers, and residents who have been in close contact with the employee will be isolated and monitored twice-daily for 14 days."
Effective Friday, all people working in long-term care facilities in Saskatchewan will have their temperatures checked and will be monitored for COVID-19 symptoms before beginning their shifts.
On a promising note, 48 out of 220 people have recovered from the virus, making for a recovery rate of 22 per cent of known cases.
Pandemic planning updates coming next week
Premier Scott Moe said Thursday that he hadasked the health authority to publicly release updated projections of how many people in the province might become infected and die from the virus, under various scenarios.
That update which will also touch on planning for field hospitals and COVID-19 care in existing hospitals is expected early next week.
"They all do fit together," Shaw said of the modelling, the operational plan and the ethical framework for decision-making.
"We want to share it," she said of the ethical framework. "It's not quite ready to be shared but it is ready to start being talked about."
'None of this can be rushed'
A front-line aspectof Saskatchewan's pandemic planning has come to light thanks to a Facebook post on Thursday.
A health care worker shared photos of herself and colleagues at Royal University Hospital clothed in face shields, gloves and full-body suits. They were practicing intubation on "Harold."
"Harold is a simulation dummy for the newly formed intubation teams to practice on," the worker wrote. "We are teams of anaesthesiologists, AAs and nurses who practice and train day or night every shift until there is a real patient with COVID-19 who cannot breathe on their own.
"I am grateful that we have this time to get prepared," the worker added.
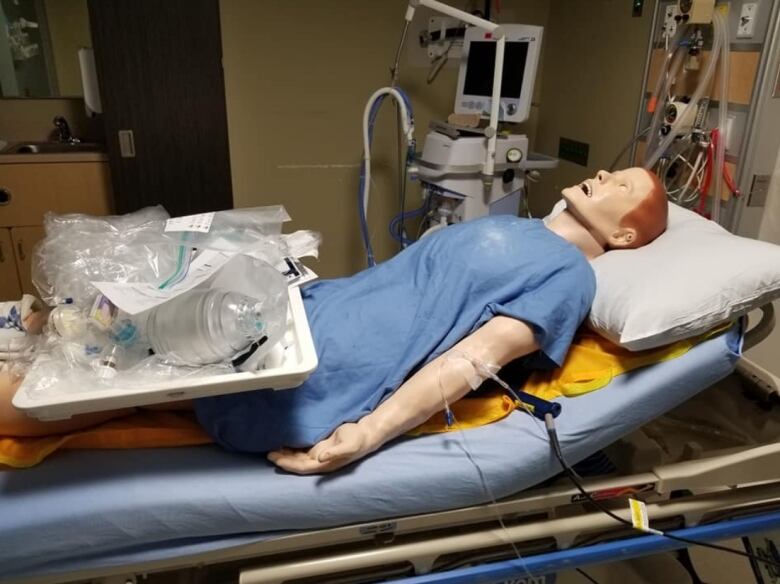
Shaw confirmed this type of COVID-19-specific training has gone on for at least two weeks.
"Putting a breathing tube in somebody is a very routine activity for an anesthesiologist and many other health care professionals," Shaw said. "But how do you do it [properly] while appropriately donning and doffing equipment?"
Shaw even joined in the exercise later on Thursday.
Spent my evening at RUH ICU with @SaskHealth anesthesia airway team practicing scenarios to safely care for #COVID19SK patients
Proud of my colleagues. We are in good hands
—@drsusanshaw"Proud of my colleagues. We are in good hands," Shaw wrote on Twitter.
'Staff safety is the number one priority'
The health care worker who posted on Facebook said putting on and taking off equipment takes a long time, but with good reason.
"So that we health care people can be as safe as we can," she wrote. "None of this can be rushed as staff safety is the number one priority."
During Thursday's provincial COVID-19 news conference, Moe saidthe procurement of more personal protective equipment (PPE) for front-line workers was his top priority on a call that same afternoon with Prime Minister Justin Trudeau and other premiers.
The health worker wrote in their Facebook post that the trainees weren't wearing N95 masks in order to "save them for when they are actually needed."
At the same provincial news conference, Shahab cited instances where it was not initially known a patient had respiratory symptoms and so health care workers were not wearing the right PPE.
Shahab said patients should always phone a clinic instead of just going there.
The health care worker training forCOVID-19 intubation had some advice too.
"You definitely don't want to become a Harold. Stay home, and stay safe."












_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)