Ontario's COVID-19 test positivity climbs to 13.5% as new details of 7th wave emerge
Hospitalizations, ICU admissions also on the rise; greatest jump in cases among children 4 and under

New details are emerging about the severity of Ontario's newest wave of COVID-19, with the province reporting another 33 deaths related to the virus over the last week, as well as rising numbers of hospitalizations and ICU admissions.
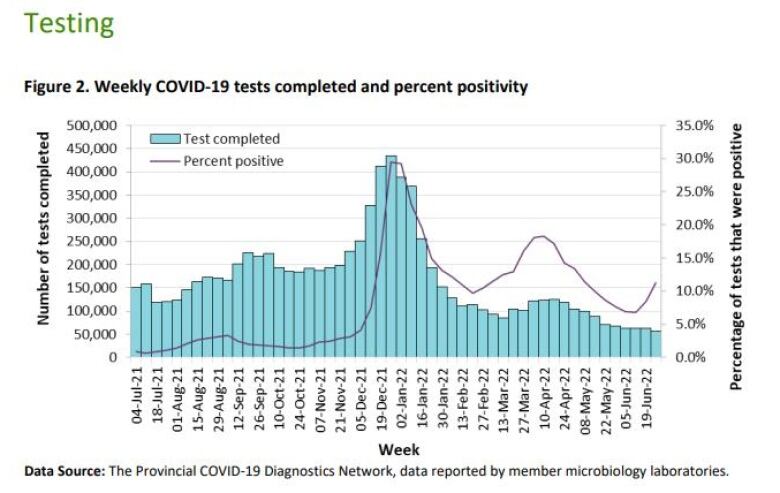
Test positivity has also climbed to 13.5, the highest percentage reported since May, it reported Thursday.
The province says 712 people are currently in hospital with COVID-19, up from 585 at this time last week. There are 110 patients in intensive care due to the virus, up from 95 last Thursday.
The new numbers come as Public Health Ontario released its latest weekly epidemiological summary, which noted the province's seventh wave of COVID-19 began as early as June 19. Ontario's top doctoronly confirmed the newest wave Wednesday, saying the province is now in its third week of the spike.
According to the summary, case rates have increased across 25 of Ontario's 34 public health units as of July 2, and in all age groups.
The biggest jump was among children aged0-4, with cases in that group spiking by 40 per cent. Case rates remain higher among those 20 and over and are still highest among those 80 and up.
While admissions of COVID-19 to hospitals and ICUs are slowly rising, Chief Medical Officer of Health Dr. Kieran Moore says he expects the ultimate impact on the health-care system to be more modest than previous waves.
The BA.5 subvariant is highly transmissible, though Moore said there is no evidence to suggest it is more severe than the subvariants responsible for earlier waves. The hope, he said,is that continued vaccinationswill keep most people who contract the subvariant out of hospital.
Ontarians under 60 still not eligible for 2nd booster
Ontario lifted its remaining mask mandates in early June, and there are no indications the province will requirethem again until possibly the fall should the strain on the health-care system grow severe enough, Moore suggested Wednesday.
Moore also said an announcement about expanded eligibility for second boosters could be coming soon, but provided no specifics.
The province's reluctance to open up fourth COVID-19 vaccine doses to more adults has drawn criticism from some health professionals.
Booster shots temporarily increase protection against severe outcomes from the illness to about 90 per cent, Moore said, but that protectionwanes month over month. By five months, protection against severe health outcomes falls to roughly 70 per cent, with theeffect even more pronounced in older people.
Around7.4 million Ontarians have already received one booster, and nearly 90 per cent of those shots were administered at least five months ago, according to recentPublic Health Ontario data.
Roughly five million people have not had a first booster shot yet, including about a million Ontarians over 50, Moore said. Meanwhile, about 1.3 million eligible Ontariansadults aged 60 and olderhave had a second booster shot.
Hospital staff morale has plummeted, says ER physician
Meanwhile, after two and a half years of thepandemic, one doctor is warning Ontario's hospital system will struggle to deal witha significant influx of COVID-19 patients, with emergency departments in particular under incrediblecontinued strain.
"I can't think of a time when morale was lower than now. People have been working full tilt for a long time now," said Dr. Kashif Pirzada, an emergency room physician in Toronto.
Pirzada told CBC Radio's Metro Morningmany hospital staff are taking early retirements or leaving the field entirely.
Emergency departments are being pushed to their breaking point amid staff burnout and shortages, as well as an increase in people seeking treatment they put off earlier in the pandemic, he noted.Staffing restraints and a COVID-19 outbreakrecently caused the temporary closure of the emergency department at thePerth and Smiths Falls District Hospital.
While the ongoing seventh wave may be less severe for hospitals, Pirzada said he's also concerned about the coming colder months when Ontarians head indoors without mandatory masking.
"This wave of COVID that we are getting right now is probably going to be lighter because of the nicer weather. But can you imagine what's going to happen in fall and winter if we still have few staff and even more burden of illness?"
In a statement to CBC News, the Ontario Nurses' Association said front-line nurses and health-care professionals "certainly do not believe that hospitals have the capacity" to cope with current patient loads, and "certainly will be challenged" by a potential surge in the seventh wave.
"One look at the state of our emergency rooms and the closures that are being announced says it all," said the statement from ONA president Cathryn Hoy.
The Ontario Hospital Association, for its part, said"very high numbers" of patients in the province's hospitals are waiting forlong-term care andhome care.
"There is no denying that these broader health system capacity pressures have a domino effect throughout hospitals. That said, while the system is under considerable pressure, hospitals are able to manage current COVID-19 pressures and will continue to be here to care for the communities they serve no matter the circumstance," said spokesperson Hannah Ward.
The association went on to say it's working with the government to make sure hospitals and other providers have as much support as possible "particularly in advance of the fall and winter when influenza and COVID-19 may return simultaneously."
With files from Metro Morning












_(720p).jpg)


 OFFICIAL HD MUSIC VIDEO.jpg)
.jpg)



























































































